Are you believing any of these 5 myths about eating disorders?
February 24th, 2020 by Sara Upson
Every year the last week of February is national eating disorder awareness week. Somehow, I’m often giving a presentation during this week (but not this year). When I ask the audience if they know that it’s national eating disorder awareness week most people don’t- and sometimes it’s even at eating disorder specific events. Everything has a week these days- but this is one that’s important to me and hopefully you too.
Eating disorders are far too common. Current research suggests that 30 million Americans struggle with an eating disorder – that 20 million women and 10 million men will have an eating disorder at some point in their life. And specifically that 10 million women struggle with anorexia nervosa (AN) or bulimia nervosa (BN) and 1 million men. Additionally 13 million men and women struggle with binge eating disorder (BED). On top of that 1 in 4 women struggle with an eating disorder or disordered eating.
Eating disorders are a lot more common than you think and there are so many myths surrounding them! Here are the top 5 myths that I see in clinical practice and just on a day-to-day basis about eating disorders.
1. Myth: You can tell if someone has an eating disorder.
Reality: You can’t look at someone and know if they’re struggling or how much. The media sensationalizes what an eating disorder look likes creating this expectation that you’ll be able to tell if someone has an eating disorder- but the truth is– you can’t tell.
You can tell nothing by looking. The media’s portrayal of eating disorders is extremely harmful because it reinforces to many people that they’re not sick enough, that they don’t have an ED, that they’re fine when they are unwell, struggling and desperately need help. I wrote an entire blog about this last week that you can read here. This belief hurts a lot of people and prevents them from getting help.
2. Myth: Only young, white women get eating disorders.
Reality: All ages, genders, races, cultures, socioeconomic statues struggle with disordered eating and eating disorders. It’s not the 80s anymore (when everyone thought that it was just young, white women) but this belief just won’t go away. Eating disorders impact ALL demographics and don’t discriminate among population groups
The scary thing is the more research we have, the more we learn that the prevalence in diverse populations is actually higher than previously thought: Historically, it was thought that:
- Men account for 1% of eating disorder cases but research is indicating it could be as high as 25% (Hudson, 2007)
- Only teenagers had eating disorders, but prevalence of eating disorders for patients aged 45-65 increased by 88%, more than for any other age group and counted for 35% of eating disorder related hospitalizations. (Zhao, 2011)
- Eating disorders only impacted individuals of higher socioeconomic status, but research indicates that 17% of individuals with food insecurity also struggle with an eating disorder. (Becker, 2017) Eating disorders have increased at a faster rate in men, lower socioeconomic, and older participants.
- Only white women struggled with an eating disorder, but research indicates that Hispanics were more likely to suffer from bulimia than non-hispanics (swanson, 2011) and that black teenagers are 50% more likely to exhibit bulimic behaviors than white teenagers. (Goeree, 2011)
The belief that only certain individuals get eating disorders prevents people from getting the help they need.
3. Myth: Eating disorders aren’t that serious.
Reality: Eating disorders have the second highest mortality rate of all mental illnesses, surpassed only by the opioid epidemic. (Chesney, 2014).
I once had a doctor friend ask what I did. When I replied that I was a dietitian that specialized in the treatment of eating disorders they rubbed their stomach and made an asinine comment about needing more control around their eating. Comments like that make me so angry! Eating disorders aren’t a choice or something to have just a “touch” of. Eating disorders impact multiple systems within your body and kill.
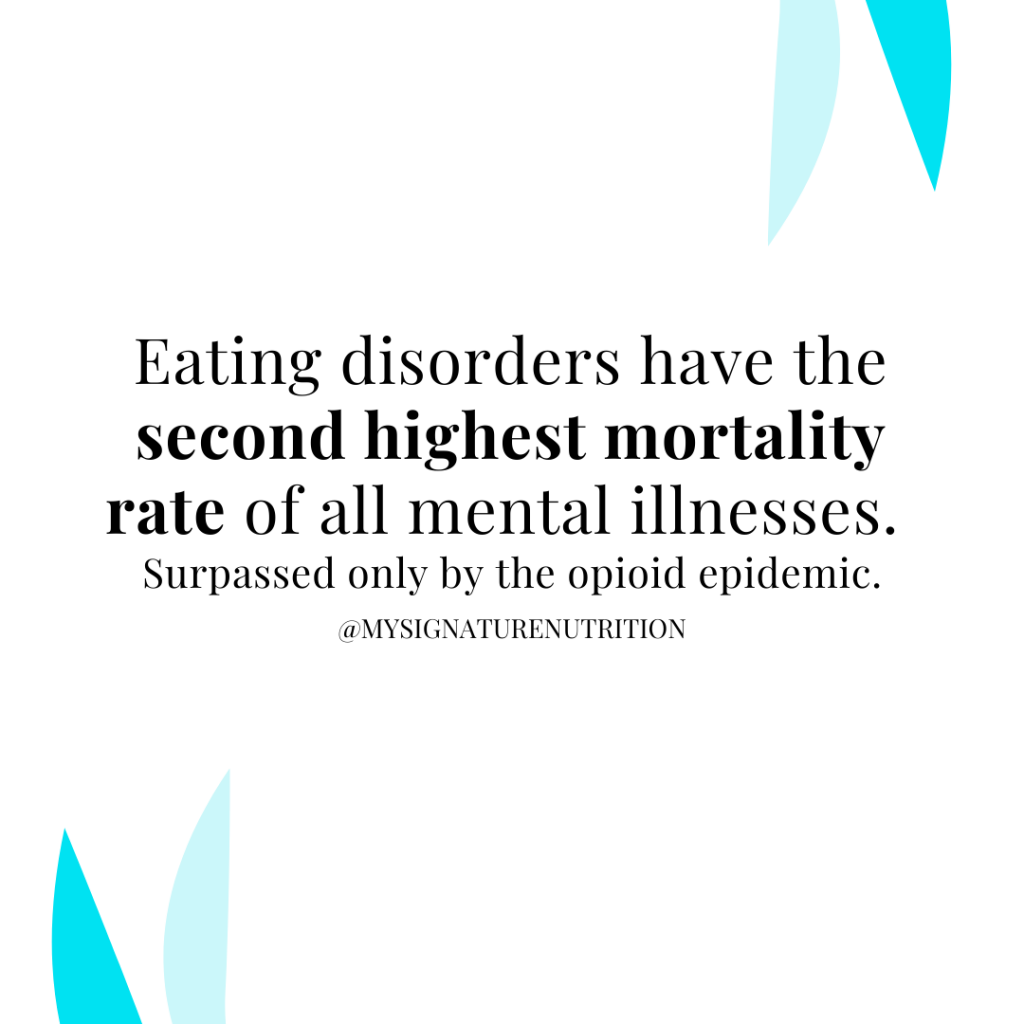
Eating disorders negatively impact health specifically the cardiorespiratory, gastrointestinal, and endocrine systems. Additionally they can lead to a wide variety of health complications including: weakness, fatigue, cold intolerance, fainting, hot flashes, hypoglycemia, chest pain, heart palpitations, orthostatic hypotension, bradycardia, shortness of breath, edema, bloating, stomach pain, reflux, hemorrhoids, constipation, amenorrhea, loss of libido, stress fractures, infertility, depression, anxiety, memory loss, difficulty concentrating, insomnia, seizures, hair loss, poor wound healing, yellowing skin, dry and brittle hair and nails.
Eating disorders are very serious and they kill. Jokes about eating disorders are completely inappropriate (it’d be like joking about cancer). Believing that you can just wait and see what happens with an eating disorder is a dangerous decision. Eating disorders are not “watch and wait” medical conditions- they’re a health crisis that requires immediate intervention and access to appropriate medical care.
4. Mtyh: Eating disorders are a choice. They should just go eat a hamburger.
Reality: Eating disorders are life threatening and life consuming. One thing that is commonly heard about eating disorders is- “just go eat a hamburger.” These comments are so frustrating! If it was as simple as eating a hamburger or some other specific food- don’t you think they would’ve done it already? Don’t you think that it wouldn’t be a serious mental illness if that was the case??? Because it’s just not that simple.
Eating disorders impact almost all areas of life and lead to isolation, withdrawl from friends and activities, mood swings, emotional instability, anxiety, preoccupation wth weight, food, calories, macros, health, food rituals, poor body image, and personality changes.
They’re not:
- a teenage phase that can be grown out of
- a lifestyle choice where someone can just choose to get better.
- Just a choice
Eating disorders are a brain based biological mental illness. Eating disorders are complex in nature and involve a range of biological, psychological, and sociocultural issues. (Also known as a bio-psycho-social model.)
Some risk factors include:
- Biological: having a direct relative with an eating disorder or other mental health condition, dieting, being in negative energy balance (burning more calories than you take in),
- Psychological: personality traits that include perfectionism, harm avoidance, rigidity, behavioral inflexibility- or following the rules, impulsivity, novelty seeking, people pleasing, anxiety, emotional dysregulation, body image dissatisfaction,
- Social: cultural messages about food and body, weight stigma, diet culture, bullying, loneliness, internalization of cultural messages, trauma.
The belief that they are a choice or phase minimizes the complexity and the seriousness of eating disorders and prevents people from getting the help they need.
5. Myth: My doctor or clinician is trained in identifying and treating eating disorders.
Reality: It’s a startling and sad reality that most health professionals- doctors including psychiatrists, nurses, therapists, and dietitians are not trained in eating disorders.
Health professionals may receive some minimal training in school- but typically it is no more than the diagnostic criteria from the DSM. For many health professionals eating disorders are an elective. Which leaves providers feeling ill equipped to recognize an eating disorder and to not hold bias against the individual (that it was a choice or their fault.)
Because of this lack of education, eating disorders are frequently misdiagnosed or overlooked. Worse than that, they’re minimized and patients are assured that they’re “healthy” and “fine.”
54% of physicians felt incompetent in treating patients with eating disorders. Furthermore, because health professionals don’t understand eating disorders they often report feeling frustrated with these patients With these statistics it’s no wonder that eating disorders are misdiagnosed or overlooked.
I personally believe that all health professionals should be educated on eating disorders and how to refer to specialists for treatment. But because this isn’t true, sadly this your doctor, pediatrician, or therapist may not be the best place to start for eating disorder treatment. The best place to start is with an eating disorder specialist- who has met specific criteria defined by the international association of eating disorder professionals to hold the certification as an eating disorder specialist.
When the front line supporters for most people aren’t trained in eating disorders, it’s just another barrier to getting help.
Since we live in a culture that promotes disordered eating, applauds weight loss at all cost, and is rampant with weight stigma, it’s no wonder that so many people struggle. In addition to changing the cultural message- we also need to be doing better at helping people get help, at raising awareness about the seriousness of eating disorders. They’ve been misunderstood and minimized for far too long which has caused years of suffering and taken far too many lives.
Sources:
Zhao, Y., Encinosa, W. Update on Hospitalizations for Eating Disorders, 1999 to 2009. HCUP Statistical Brief #120. September, 2011. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb120.pdf
Hudson, J., Hiripi, E., Pope, H., & Kessler, R. (2007) “The prevalence and correlates of eating disorders in the national comorbidity survey replication.” Biological Psychiatry, 61, 348–358.
Goeree, Michelle Sovinsky, Ham, John C., & Iorio, Daniela. (2011). Race, Social Class, and Bulimia Nervosa. IZA Discussion Paper No. 5823. Retrieved from http://ftp.iza.org/dp5823.pdf.
Swanson SA, Crow SJ, Le Grange D, Swendsen J, and Merikangas KR. (2011). Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 68(7):714-23.
Chesney, E., Goodwin, G. M., & Fazel, S. (2014). Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry, 13(2), 153-160.
Comments are closed.